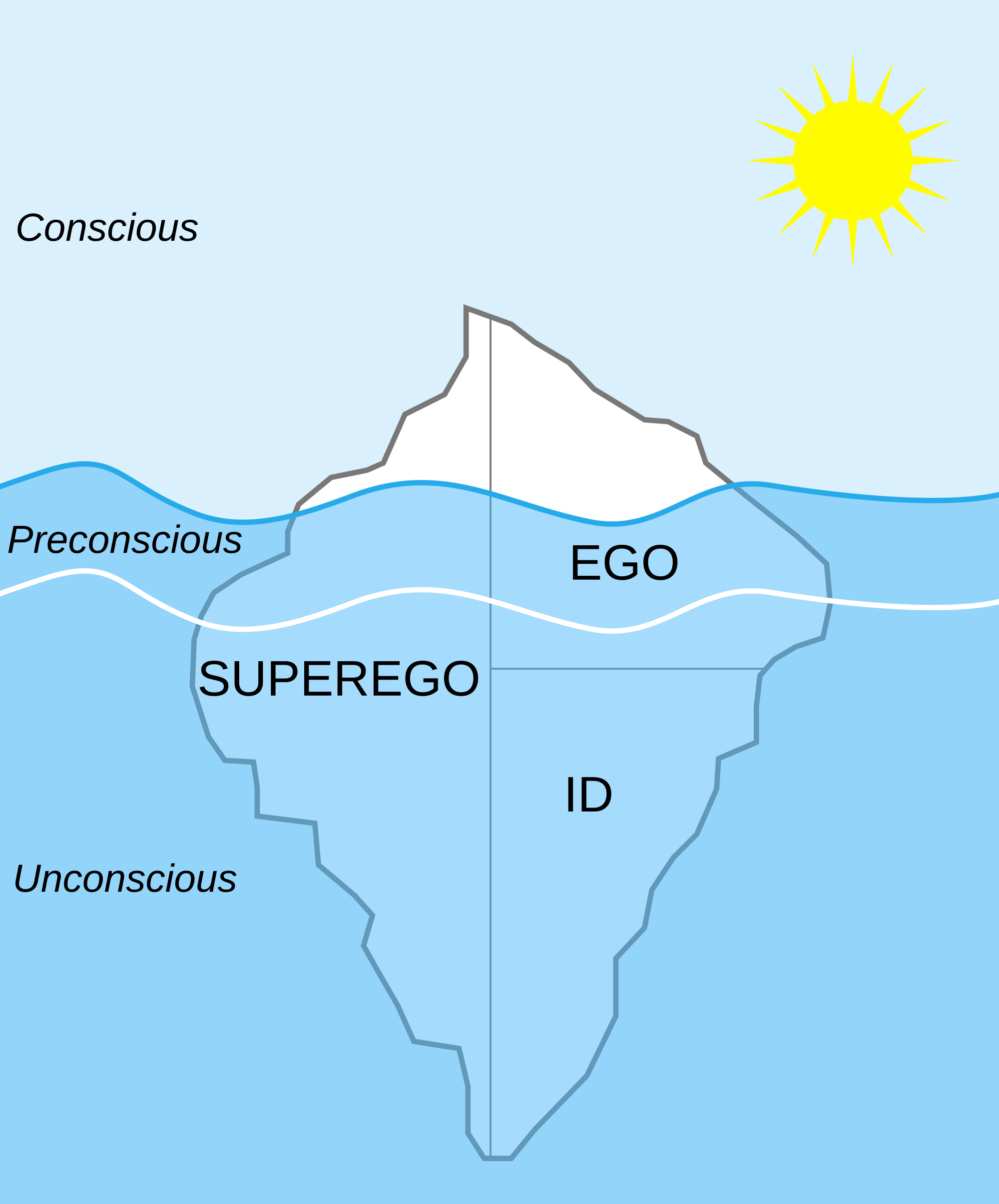
“Tell me your story,” I like to say, which leads to a confused look. “The whole story?” A 20-year-old patient named Libby responds. I think 20 years is not that much, but to her, she thinks the summary of her life is an impossible task. The open-ended question is designed to see where the patient will begin. Will she tell me where she was born, whether her parents stayed married, or will she focus on her friends or her academic life. As she constructs a narrative, it is my job to formulate hypotheses about why she is in my office. Of course there is the stated reason she came, but there are many unstated, and unknown reasons she is there as well. I am looking for, what some authors would term, “the analytic surface,” which means where to take her narrative and go deeper. Libby spent a great deal of time talking about her mom leading me to think her parents were divorced, but in fact they were not. This confusion of mine leads me to wonder if perhaps Libby wished they were divorced, and/or felt neglected by her dad and controlled by her mom. “What about your dad?” I ask, intruding into her narrative since my sense was that the absence of hearing about her dad was meaningful. “He was there and he was not there. He did not seem to care about us,” she says with tears in her eyes. The analytic surface in this case was a large and lengthy discussion of her relationship with her mom, moving us to the seemingly more painful relationship with her dad. Struggling to work with this analytic surface is the art of psychotherapy in that from this surface I try to look for meaningful experiences which are harder for us both to see, at first glance. This digging, if you will, needs to be gentle so as not to overwhelm the patient, but it also needs to penetrate the conscious experiences so the patient can experience her life in a deeper and more liberating way. Going below the analytic surface helps the patient understand the inhibitions and constrictions which prevent her from embracing her life.




